Implanted Heart Rhythm Devices
APR 08, 2024A healthy lifestyle is very important to protect the electrical system of the heart. Once it gets damaged, the heart may have little ability to recover.
Read More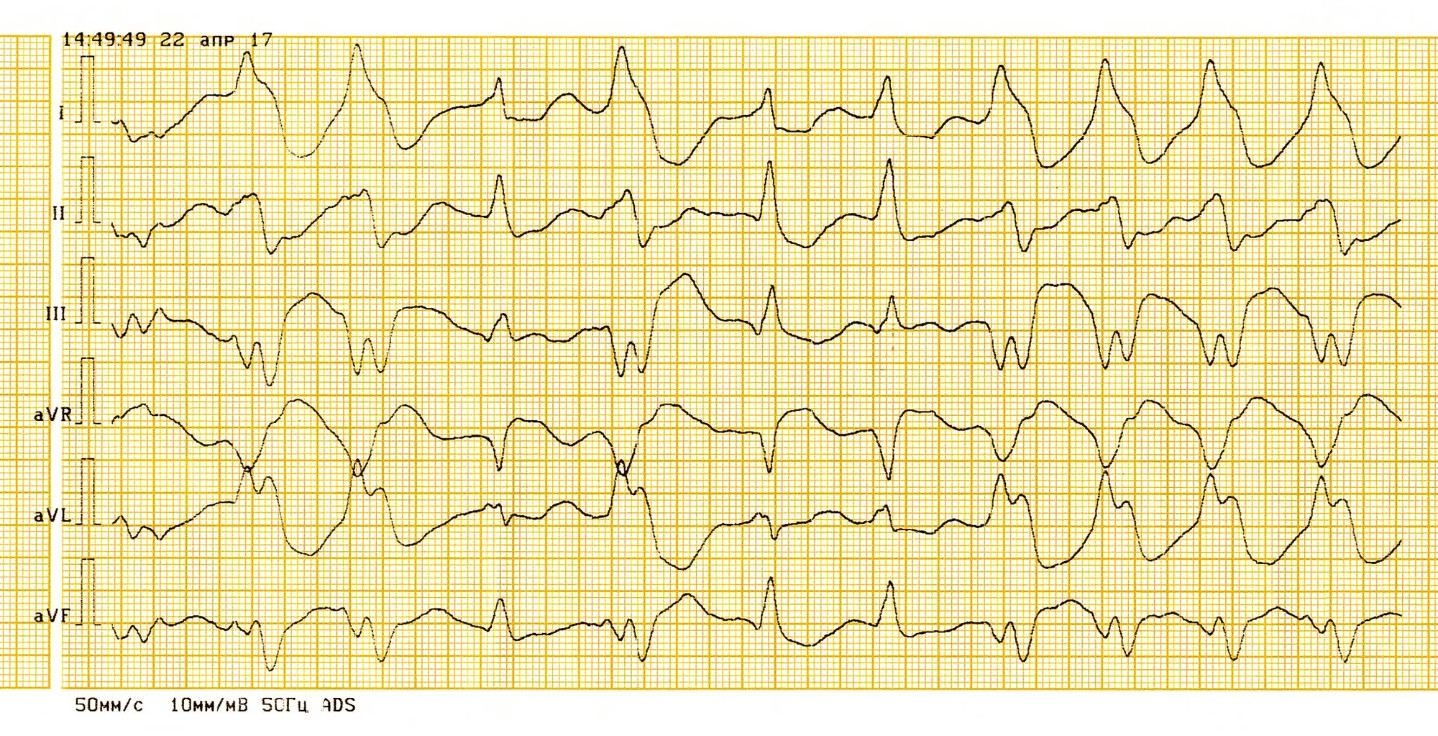
At least once a week I get a consult for palpitations. Since this is such a common problem, I thought it might serve as a good subject to write about.
If we define palpitations as the abnormal sensation of one's own heart beat, then I would propose that everyone has palpitations at some point in their lives. The most common descriptions I hear are the sensations of irregular or skipped beats, pounding in the chest, flip-flopping of the heart, or just the simple "awareness" of a regular heart beat.
Palpitations can affect patients of all ages, though I think it's more often present in younger people. For some reason, older patients can have remarkably irregular heart rhythms and feel little or no symptoms.
By far the most common cause of episodic palpitations is the presence of premature atrial (PACs) or ventricular contractions (PVCs). Virtually everyone has these occasionally. It is relatively uncommon to see a patient who can wear a 24-hour continuous ambulatory heart monitor (Holter monitor) and not exhibit at least a couple PACs or PVCs in a day. These are almost always benign.
Only rarely is the presence of premature beats a marker for a more serious underlying structural or functional problem that could put the patient's health at risk. Previously unidentified problems such as atrial septal defect or cardiomyopathy could produce palpitations as their initial symptoms. These can be easily screened with an echocardiogram.
An electrocardiogram (ECG) is useful but will be normal in most people. In a small subset of patients we'll pick up sustained arrhythmias such as atrial fibrillation or flutter. The substrate for a few very rare life-threatening arrhythmias can also show up on resting ECG.
The Holter 24-hour monitor is often the next evaluation. The patient wears a monitor for a day and every single heartbeat for that period is recorded and analyzed. The 24-hour monitor has several limitations, though.
My experience is that most patients with frequent and severe palpitations will enjoy the quietest 24 hours they've had in weeks. In physics, this phenomenon is called the "observer" or "Hawthorne effect," but I prefer to call it the "bring-your-broken-car-to-the-shop-and-watch-it-work-like-brand-new-when-the-mechanic-starts-it effect," for obvious reasons.
If the Holter monitor doesn't provide enough information--and if the patient hasn't yet had their fill of stickers on the chest--we also have other monitors that can be worn for up to a month.
Since palpitations due to PACs and PVCs are universally benign (as long as the resting ECG and echocardiogram are normal) the question arises: do we need to treat them? The answer depends on the patient.
For significantly symptomatic patients I start with a low dose of a beta-adrenergic blocking drug (beta-blocker). This class of medication essentially decreases the effect of adrenaline on the heart and can blunt the symptoms that accompany the abnormal heart beats. If the palpitations are nothing more than a nuisance, then perhaps the knowledge that they don't portend anything ominous is all the patient needs. Most patients in my clinic prefer to not take medication every day (with associated possible side effects) in order to treat something that poses no risk.
For a very few, the palpitations can be truly miserable and disrupt their quality of life. In most cases, we can provide some measure of relief with beta-blockers or other, more aggressive, medications. The good news is that most young symptomatic patients will eventually "outgrow" this problem and the palpitations will fade away as the years progress. Also, the presence of frequent PACs or PVCs is not a contraindication to exercise, since most patients will have fewer premature beats as their heart rate increases.
In summary, I evaluate the patient with palpitations with an ECG and an echocardiogram to screen for rare underlying problems. I ask for a 24-hour monitor on only the most symptomatic patients who have frequent episodes. Thankfully, most palpitations in young, otherwise healthy individuals arise for benign reasons and require no treatment except the knowledge that this isn't a dangerous problem.

A healthy lifestyle is very important to protect the electrical system of the heart. Once it gets damaged, the heart may have little ability to recover.
Read More
Heart disease is the number one cause of death for women and men, claiming more lives than all forms of cancer combined.
Read More
With heart disease remaining the number one killer of women and men in the United States, it’s important to take action to protect your heart – even if you feel fine.
Read MoreWhen you need local health information from a trusted source, turn to the CHI Health Better You eNewsletter.