
Breaking Boundaries: Teamwork Triumphs in Advanced Melanoma Case
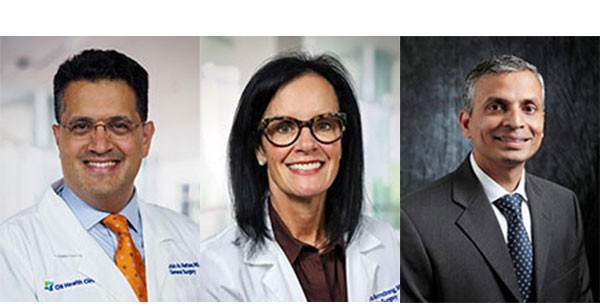
Left to right: Dr. Waddah Al-Refaie, Dr. Deanna Armstrong, Dr. Nagendra Natarajan
Collaboration and innovation have transformed the life of a patient with advanced melanoma. A team of specialists including CHI Health Chair of Surgery Dr. Waddah Al-Refaie, CHI Health plastic surgeon Dr. Deanna Armstrong and Dr. Nagendra Natarajan navigated the complexities of the case to achieve a milestone in melanoma treatment. Dr. Al-Refaie provides a detailed look into the collaborative efforts and innovative strategies that led to a remarkable outcome.
As part of our multidisciplinary melanoma and soft tissue oncology team, Drs. Al-Refaie, Armstrong, and Natarajian collaborated and managed a complex case of advanced Stage IIIC melanoma metastasis to the inguinal region. Over three years ago, this multi-morbid patient was surgically-treated with wide local excision of an acral melanoma and negative sentinel lymph node biopsy. The patient presented with biopsy-proven melanoma nodal relapse in the absence of radiographic evidence of distant metastatic disease. Pre-therapy molecular profiling revealed low tumor mutational burden, absence of BRAF, NF1. After discussing the case at our multidisciplinary tumor board conference and reviewing pre-referral histologic slides, the consensus decision was to proceed with pre-operative Pembrolizumab followed by radical resection and therapeutic nodal dissection (as per SWOG1801 trial). After 3 cycles of pre-operative Pembrolizumab, staging cross-sectional imaging showed stable to possible radiographic pseudo-progression raising open questions about progression vs. pseudo-progression due to underlying treatment-related necrosis. There was no radiographic evidence of distant metastatic disease.The patient underwent therapeutic inguino-femoral nodal dissection, radical resection of thigh mass, with immediate reconstruction. In line with known high risk for postoperative surgical site infection, the reconstruction of the defect required a sartorius flap to cover the femoral vessels. Advancement flaps were also used to decrease the size of the large defect. Finally a large skin graft was used to complete the reconstruction. A wound VAC was placed over the entire repair to ensure stability of the closure. The patient pathology report showed margin-negative resection, matted adenopathy, and extensive necrosis. Given high risk of recurrence with Stage IIIC melanoma, the patient will undergo adjuvant immunotherapy, ct-DNA levels measurement, and close staging surveillance.
For questions about complex melanoma cases, contact Dr. Al-Refaie via email at: [email protected] or [email protected] or call (402) 717-4900 or (402) 717-4830.